Gm case(60 yr male)
GENERAL MEDICINE
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and prognosis
DATE OF ADMISSION- 12-4-2023
A 60 year old male resident of marepally farmer by occupation came to the OPD with the chief complaints of
CHIEF COMPLAINTS:
Burning mituration on and off since 2-3months
Burning sensation near heart since 5 days.
Bilateral pedal edema since 5 days.
Shortness of breath since 5 days
HISTORY OF PRESENT ILLNESS : patient was apparently asymptomatic 4 years back then he developed lower back pain which was in sudden in onset gradually progressive no aggregating and reliving factors and no associated symptoms.
Then he went to hospital where they diagnosed it as kidney failure and on medication since then.
Then 5 days back, he complained of pedal edema which was insidious in onset gradually progressive grade 1 pitting type no aggregating and reliving factors.
Associated with pain in the legs while walking.
Shortness of breath since 5 days grade 3 which is sudden in onset gradually progressive aggravated on walking relieved on taking rest not associated with fever.
Burning sensation in the chest near the heart since 5 days sudden in onset.
History of burning mituration on and off since 2-3 months not associated with fever
No history of PND,orthopnea, nausea, vomiting, giddiness,generalised weakness
PAST HISTORY-
No similar compliants in the past
Known case of diabetes since 8 years.
Known case of hypertension since 6 months.
No history TB,asthma,CHD,CVD,eplipsy.
No drug allergies.
Family history : not significant.
PERSONAL HISTORY
Sleep : adequate
Diet : mixed
Appetite : normal
Bowel and bladder movements : regular
Smoking and alcohol stopped 2 months back.
GENERAL EXAMINATION-
Patient is conscious, coherent , cooperative well oriented to time, place and person.
Moderately built and nourished.
Pallor : mild
Icterus : absent
Cyanosis : absent
Pedal edema : present grade 1
Lymphadenopathy : absent
VITALS-
BP : 130/80mm of Hg
Pulse : 86/min
RR : 8/min
Temperature : 98.8F
Spo2 : 97%
GRBS :108 mg%
SYSTEMIC EXAMINATION-
.Respiratory system examination :
1.Inspection :
Position of trachea central
No dropping of right shoulder
No intercostal indrawing
No supraclavicular hallowness
Shape and symmetry of the chest normal.
No dilated veins.
No visible scars.
accessory muscles of respiration not prominent.
2.Palpation :
On three finger test : position of the trachea central.
Respiratory movements are normal
Measurement of left and right hemithorax :
Antero posterior diameter :
Transverse diameter at the level of nipples :
AP/transverse diameter ratio =
Distance between vertebrae and infrascapular angle on right and left side is same =
Vocal framitus :. Right. left
Supraclavicular area. N. N
Infraclavicular area. N. N
Mammary area. N. N
Axillary area N. N
Infraxillary area N N
Suprascapular area. N. N
Interscapular area. N. N
Infrascapular area. N. N
3.Percussion :
On direct percussion in clavicular area :
Tidal percussion: resonant note in the right 5 th intercostal space after deep inspiration.
Traubes space percussion : dull note
4.Ascultation :
Vocal resonance :
Right left
Supraclavicular area. N. N
Infraclavicular area. N. N
Mammary area. N. N
Axillary area N. N
Infraxillary area N. N
Suprascapular area. N. N
Interscapular area. N. N
Infrascapular area. N. N
Normal vesicular breath sounds.
Bilateral air entry positive.
No crackles heard.
. On abdominal examination:
1.Inspection:
Shape of abdomen is scaphoid
Flanks are free
Umblicus is in position, inverted
Skin over abdomen normal shiny, no scars, no sinuses, no nodules, no puncture marks.
No visible veins.
No engorged veins.
Movements of abdominal wall are normal, no visible gaatric peristalsis.
2.Palpation:
Liver examination:
.On superficial palpation
no tenderness , no raised temperature
.On deep palpation
No tenderness in liver
Non pulsatile
.Spleen examination:
No tenderness and pain
3.Percussion :
No fluid thrill.
No shifting dullness.
Percussion of Liver for Liver Span : 14cm
4.Auscultation
Normal bowel sounds heard.
2. Bruit - no renal artery bruit heard.
no iliac artery bruit heard.
CVS Examination :
1.Inspection :
No abnormal palsations
No visible scars.
No chest deformities.
Mediastinum normal
Trachea central in position.
2.Palpation :
Mediastinal position : apex beat normal
Position of trachea central.
3.Percussion :
On percussion No cardiomegaly.
4.Ascultation : on examination of mitral area, pulmonary area, tricuspid area and aortic area S1 and S2 heard. No murmurs heard.
CNS : NAD
PROVISIONAL DIAGNOSIS-
CHRONIC KIDNEY DISEASE
CLINICAL IMAGES
INVESTIGATIONS
Complete blood picture
Complete urine examination Anti HCV antibodies
Serum iron
Uric acid serum
Serum electrolytes Serum creatinine
Blood urea
Blood sugar random
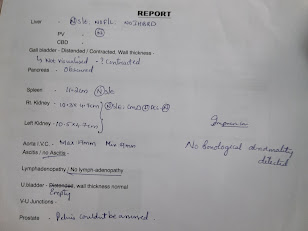
Usg abdomen
TREATMENT


















Comments
Post a Comment